What is Venous Reflux?
The Venous Reflux test is used to determine the competence of the superficial venous valves in the calves of the legs. This test is performed with a DC PPG(photoplethysmography) sensor.
When the venous valves are not functioning properly, they may “leak”, resulting in a reversal of blood flow in the veins. In turn, this problem causes improper venous blood return and pooling of blood in the veins of the legs, which may result in a variety of venous insufficiency disease. The Venous Reflux test is a common non-invasive diagnostic examination designed to determine the venous vein valves’ competence in the lower part of the legs.
How to Perform Venous Reflux Test
During a typical Venous Reflux examination, the patient is requested to sit upright. In some protocols, the patient’s feet do not touch the floor, while in other protocols, the feet are flat on the ground. A Photoplethysmograph (PPG) sensor is attached to each leg above the ankle in the posterior tibial artery region, and the patient is asked to sit still without moving the legs.
Once a steady baseline DC PPG signal is obtained, the patient is asked to perform multiple rapid leg dorsiflexions resulting in “pumping” and emptying all of the venous blood in the upward direction. When the feet are in the air and off the ground, both dorsi- and plantarflexions of the feet are possible for more effective emptying of the venous blood in the calf. The number of dorsiflexions varies between institutes and is frequently 10.
During the dorsiflexions of the feet, the venous blood in the veins is driven in the proximal direction towards the heart, and this causes the PPG signal, which represents the blood in the veins, to drop sharply. Immediately after completing the dorsiflexions of the feet, the patient is requested to remain still without moving the feet to allow to refill the veins in the legs with blood. As a result of the refilling of the veins, the PPG signal returns back towards the initial baseline.
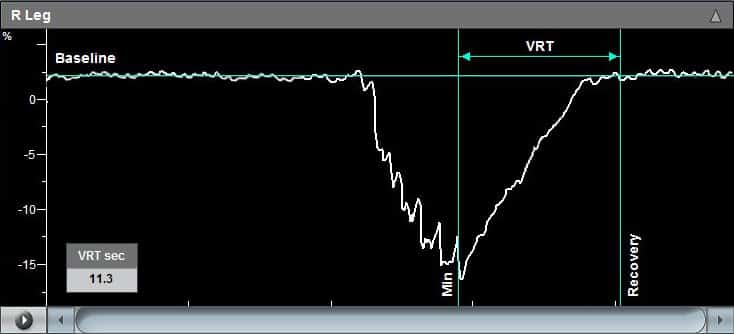
The duration from the end of the dorsiflexions (maximal PPG signal drop) and until the signal return to baseline is called the Venous Recovery Time (VRT), which is a strong indication of the status of the valves. A slow recovery time indicates competent valves, while a fast VRT suggests a suspicion of possible incompetency of the venous valves.
If the venous reflux test indicates suspicion of venous insufficiency, then a venous tourniquet can be applied at various positions above or below the knee to discriminate between deep and superficial vein valve incompetency.
PPG Disk
Color Coded High Quality PPG Sensors

Inflatable Cuffs
High quality available in a variety of sizes
Using the Falcon for Venous Reflux Test
The Falcon is designed with a dedicated Venous Reflux Test protocol to allow a fast, simple, and effective diagnosis. The Falcon disk PPG sensor is attached using a special double-sided adhesive sticker to the proper location on the lower calf. The Falcon Venous Reflux protocol then guides the examiner through the simple steps that need to be taken to complete the test effectively. These steps include:
- Obtaining a steady-state PPG signal,
- Placing an automatic signal “baseline” cursor
- The patient starts the vigorous dorsiflexions and/or plantarflexions.
- Once the vigorous foot movements are stopped, and the patient is still again, the PPG signal starts to rise towards the baseline, and an automatic time-cursor is placed at the point of minimal PPG signal value.
- Finally, once the drifting signal crosses the initial baseline value, the “Recovery” time cursor is placed at that location. The VRT parameter – Venous Refill Time – is automatically displayed as the time difference between the minimum PPG signal and the point of recovery.
The examiner or physician has the option to relocate and move the time cursors to adjust the VRT parameter per their understanding or in the event that the PPG signal did not fully recover back to baseline.
The diagnosis of the Venous Reflux test is quantitative and is based on the value of the VRT parameter.
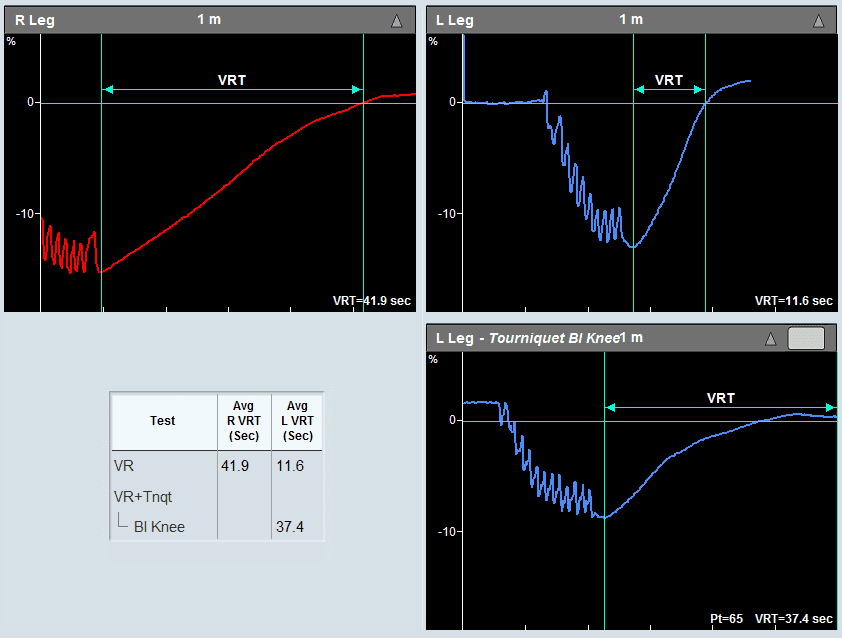
The Falcon allows to extend the VR test protocol based on the VRT findings and add a tourniquet pressure cuff that is placed on the leg, typically above and below the knee. The examiner can set the tourniquet venous occlusion pressure. The venous reflux test can be repeated with the tourniquet cuff to determine deep or superficial vein valve incompetency.
Expected Results
The diagnosis of the Venous Reflux test is quantitative and is based on the value of the VRT parameter. Typically, a VRT value greater than 20 seconds is considered normal, while a VRT value lower than 20 seconds indicates venous reflux and possible venous vein valve insufficiency.
The application of avenous tourniquet aids in the discrimination between deep and superficial vein valve insufficiency. If an abnormal VRT value becomes normal with the application of a superficial tourniquet, this may indicate that isolated superficial reflux is present. However, if the VRT value does not improve, then either deep venous reflux is present, or both superficial and deep venous reflux is present.
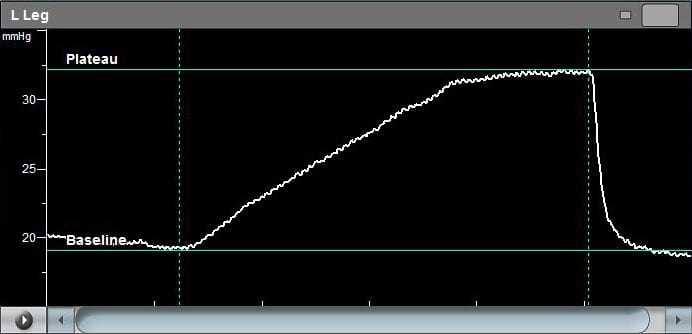
Example of a Venous Reflux specialty test performed on a patient with Viasonix Falcon/PRO. The Venous Recovery Time (VRT) is an index of venous vein valve patency. A fast recovery time such as in this example, indicates a suspicion of valvular incompetency.
Selected Literature
Diagnostic evaluation of chronic venous insufficiency, Patrick C Alguire and Barbara M Mathes, Official reprint from UpToDate, 2017
Photoplethysmographic Venous Refilling Times Following Ultrasound Guided Foam Sclerotherapy for Symptomatic Superficial Venous Reflux: Relationship with Clinical Outcomes, Darvall et al., Eur J Vasc Endovasc Surg (2010) 40, 267e272
Peripheral vascular disease assessment in the lower limb: a review of current and emerging non‑invasive diagnostic methods; Shabani Varaki et al, BioMed Eng OnLine (2018) 17:61
Ultrasound Diagnosis of venous Insufficiency, Marsha M. Neumyer, in “Introduction to Vascular Ultrasonography”, Ed. Pellerito and Polak, Elsevier Health Sciences, 2012, Ch 24, pp 408-428
Maximum Venous Outflow / Segmental Venous Capacitance (MVO/SVC)
The MVO/SVC test (Maximal Venous Outflow / Segmental Venous Capacitance) is a specific functional physiological lower limb venous test that helps diagnose obstructions to the venous circulation in the legs.
How to Perform MVO/SVC Test
The MVO/SVC test is quite simple and aims to determine the existence of venous outflow obstruction in the lower limb. The patient lies in a supine position with the legs slightly elevated. One pressure cuff is wrapped around the thigh, and a second pressure cuff is wrapped around the calf. The thigh cuff serves for venous circulation occlusion (inflated to about 60 mmHg), while the cuff that is placed around the calf is inflated to low pressure (around 20 mmHg) and serves as a sensor to detect limb circumference changes as a result of venous blood accumulation or emptying.
When the thigh cuff is inflated to venous occlusion pressure, the venous blood starts to accumulate in the lower leg, and the sensor cuff starts to show an increase in pressure.
The pressure steadily increases until a steady-state baseline is reached. The magnitude of increase from control to the baseline represents the capacitance ability of the venous circulation in the leg and is called SVC, or Segmental Venous Capacitance. Once a plateau is reached, the occluding thigh cuff is rapidly deflated. The pressure in the sensor cuff also rapidly returns back to the initial control levels. The magnitude of pressure fall in the calf cuff from the plateau level within a predefined time period, normally 1-3 seconds from thigh cuff deflation, serves as the MVO, or Maximal Venous Outflow.
If there is an obstruction to venous outflow, such as severe edema, then the venous emptying from the plateau level will take longer. As a result, MVO will decrease, and the MVO/SVC ratio will also decrease compared to normal values.

Inflatable Cuffs
High quality available in a variety of sizes
Using the Falcon for MVO/SVC Test
The Falcon has a dedicated MVO/SVC test protocol. This protocol guides the user throughout the various examination steps. It supports both unilateral or simultaneous bilateral measurements, as well as performing the test multiple times for improved accuracy.
Both the sensing cuff pressure and the venous occlusion pressures can be configured and defined by the examiner. In addition, Zoom in and out options in both the time scale and the waveform amplitude scale are available for improved diagnosis. Particularly, the program displays in detail the rapid deflation process and the corresponding fall in pressure.
In order to meet various institutional criteria, the Falcon allows configuration of the MVO calculation time, which can be set between 1 second and up to 5 seconds. Automatic cursors are placed once the thigh cuff is inflated and then rapidly deflated to mark the control baseline and the plateau levels, correspondingly. These cursors can be adjusted manually by the examiner.
The values of MVO, SVC, and MVO/SVC are automatically calculated and displayed separately for each leg. Alerts can be configured in order to help identify borderline circulation problems.
Expected Results
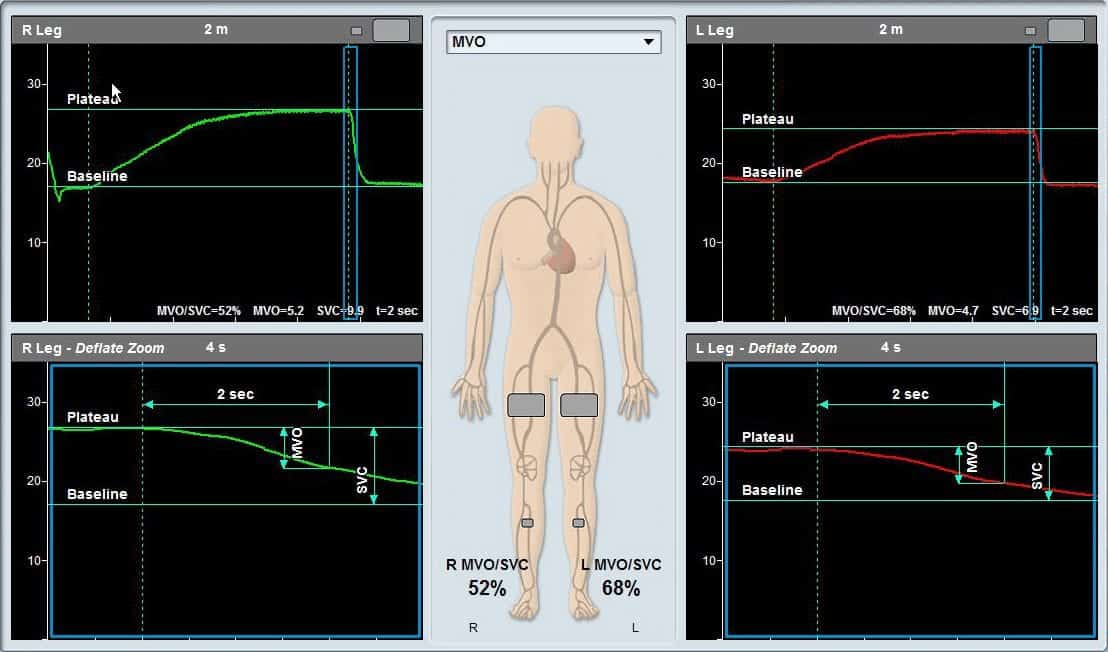
It is expected that when obstruction to venous flow in the legs exists, for example, edema, then the MVO/SVC ratio decreases. It is estimated that an MVO/SVC ratio below 50% indicates a problem.
Example of a Bilateral Maximum Venous Outflow (MVO)/Segmental Venous Capacitance (SVC) specialty test measured with Viasonix Falcon/PRO. Both legs were measured simultaneously. The top graphs show the complete measurements and the graphs below present a zoom-in on the deflation part (blue rectangle). The resulted MVO/SVC ratio is displayed on the schematic picture.
Selected Literature
Venous capacitance and venous return in young adults with typical vasovagal syncope: a cross-sectional study, Udi Nussinovitch et al., J Investig Med. 2021 Sep 27
Venous volume displacement plethysmography: Its diagnostic value in deep venous thrombosis as determined by receiver operator characteristic curves, Kevin J. McBride et al., Cardiovascular Diseases, Volume 8 Number 4 December 1981, pp 499-508





