- Patent Foramen Ovale (PFO)
- VMR / Autoregulation
- Breath Holding Test
- Brain Death Diagnosis
- Sickle Cell Disease
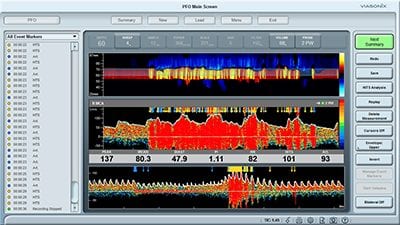
Patent Foramen Ovale (PFO)
PFO is a hole between the left and right atriums of the heart, which creates a right to left shunt for blood flow. This hole typically exists before birth, but it most often closes shortly after birth. If the hole fails to close naturally after birth, it is referred to as a Patent Foramen Ovale (PFO).
Embolism through a Patent Foramen Ovale (PFO), can be a significant cause of stroke in young adults. Transcranial Doppler is one of the preferred modalities for quick and non-invasive identification and assessment of PFO, also known as a “Right-to-Left Shunt”.
The PFO test with TCD is often called a “bubble test”, “bubble study”, or “agitated saline” because it involves the intravenous injection of micro-bubbles (air mixed saline). Along with the injection, the Doppler signal is recorded with a TCD system, most often in the Middle Cerebral artery (MCA).
In the event of an existing Patent Foramen Ovale, the injected air bubbles that are actually microemboli pass through the hole from the right heart to the left side through the open shunt. Therefore, the blood which is pumped out of the heart includes a mix of these air microemboli and reaches the cerebral circulation.

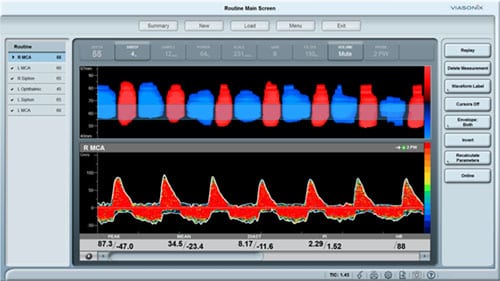
VMR / Autoregulation
Vasomotor reactivity (VMR) and autoregulation define the physiological compensatory mechanisms when flow is impaired. Identification of exhausted VMR can be a good indication for high risk for stroke.
VMR can be assessed with TCD under two specific conditions: hypercapnia or CO2 reactivity, and with intravenous injections of Acetazolamide or the Diamox test. Note that the Diamox test is not accepted in some countries.
Typically, an increase in peak velocities above 40% during induced increase in CO2 reflects intact VMR, whereas a smaller increase reflects different degrees of impaired VMR. Absence of flow increase reflects a complete exhaustion of the autoregulatory capacity.
The Viasonix Dolphin is ideal for determining the autoregulatory capacity of the cerebral circulation of patients, with dedicated Unilateral and Bilateral protocols predefined in the software. Doppler waveforms are captured automatically during baseline, and peak (hypercapnia) and minimal (hypocapnia) flows for immediate evaluation, as well as a display of the blood flow fluctuations during the entire test process. The respective parameters are automatically shown in a dedicated table with the VMR index readily displayed.
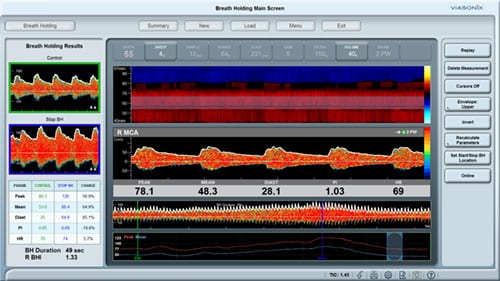
Breath Holding
The Breath Holding (BH) test is a specific test for evaluation of Vasomotor Reactivity (VMR) and cerebral autoregulatory capacity.
Identification of exhausted VMR can be a good indication for high risk for stroke. The 3 main methods to induce and test the VMR capacity include:
- The CO2 Reactivity Test, which requires installation and operation of a special CO2 hookup,
- Acetazolamide Testing, which requires intravenous (IV) medication, and
- The Breath Holding Test, which is a simple and non-invasive test that can be performed on any patient that is capable of holding a breath for at least 30 seconds.
Brain Death Diagnosis
Brain Death, or Cerebral Circulatory Arrest, is the irreversible complete loss of brain function. This condition of brain damage is characterized by almost no volume blood flow to the brain and very high distal resistance to arterial flow. This flow pattern indicates that there is no net movement of blood through the arteries of the brain, with the same volume of blood effectively shunting back and forth during each cardiac cycle, which is consistent with brain death.
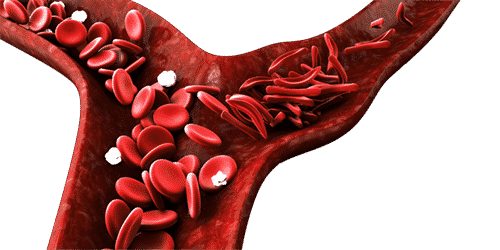
Sickle Cell Disease
Sickle Cell Disease (SCD) is a disorder of the blood caused by abnormal hemoglobin, which causes distorted (sickled) red blood cells. It is associated with a high risk of stroke, particularly in the early years of childhood.
The main risk of Sickle Cell Disease is the potential for vascular constriction or occlusion, which may lead to subclinical infarction, acute stroke, and hemorrhage. Children before the age of 20 with SCD are particularly susceptible and are at high risk of developing ischemic stroke. Blood transfusion in these cases can help to reduce the risk of stroke significantly.





