Peripheral Vascular Disease – Facts and Information
23 January 2021
Any patient suffering with hypertension carries a higher risk for renal diseases. In the first phase, the patient’s body shows almost no symptoms of renal diseases. If avoided or not taken care of, the disease reaches the second stage that makes the patient suffer renal insufficiency. The person loses around 75 percent of glomerular function and might start feeling the renal disease effects like mild hyperkalemia or anemia. If proper care isn’t rendered at this stage as well it can lead to the next stage that may lead to development of chronic renal failure.
The basic reason behind all these problems is vascular resistance in sclerosed vessels that pressurizes the blood to enter glomerulus with high speed causing severe damage to the glomerular membrane. The injured membrane loses all its ability to filter entering elements and leads to necrosis of tubules. Hypertension also disturbs the reninangiotensin-aldosterone system causing ischemia and low supply of blood volume to kidneys. Sodium and water re-absorption increases to enhance the glomerular filtration rate leading to higher vascular pressure and volume overload that causes sclerosis in the glomeruli.
The term peripheral vascular disease (PVD) is commonly used to refer to peripheral artery disease (PAD), meaning narrowing or occlusion by atherosclerotic plaques of arteries outside of the heart and brain. Risk factors for peripheral artery disease include elevated blood cholesterol, diabetes, smoking, hypertension, inactivity, and overweight/obesity.
People who suffer from peripheral artery disease are usually over the age of 50.The symptoms of peripheral artery disease depend upon the location and extent of the blocked arteries. The most common symptom of peripheral artery disease is intermittent claudication, manifested by pain (usually in the calf) that occurs while walking and dissipates at rest.
After taking a patient’s medical history and performing physical examinations, doctors may use non-invasive haemodynamic tests including segmental pressure measurements, pulse volume recordings, and Ankle Brachial indexes. Your doctor may also arrange an activity stress test alongside an ankle brachial file and heartbeat volume recording. Amid the test, the patient activities until he creates critical claudication. At that point an ankle brachial record is performed by taking systolic blood weights in the lower leg and arm all the while. Serious claudication causes a noteworthy distinction between the lower leg and brachial blood weights amid low-level activity. Pulse volume recordings are recorded in the meantime as the ankle brachial index. In the event that the patient has noteworthy impediments, the volume’s magnitude will be reduced, and the stature of its shape will be diminished.
Further examinations may include Doppler ultrasound and angiography if required to aid in the diagnosis of peripheral artery disease.
Peripheral artery disease can be treated by lifestyle alterations, medications, angioplasty with or without stent, and surgery. A combination of treatment methods may be used.
Complications of peripheral artery disease include sores that do not heal, ulcers, gangrene, or infections in the extremities. In some cases, amputation may be necessary.
Having peripheral artery disease usually indicates the potential for arterial disease in other parts of the body, such as the coronary arteries in the heart and cerebral arteries in the brain.
What is atherosclerosis?
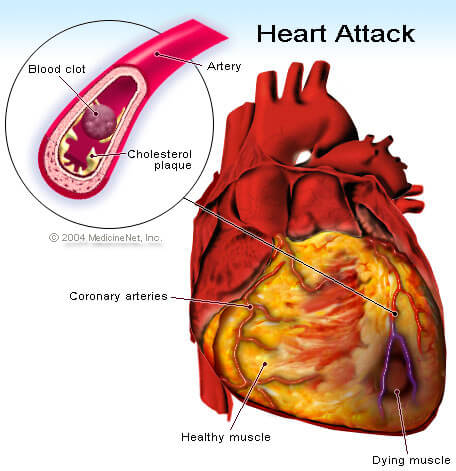
Atherosclerosis is a gradual process whereby hard cholesterol substances (plaques) are deposited in the walls of the arteries. Cholesterol plaques cause hardening of the artery walls and narrowing of the inner channel (lumen) of the artery. The atherosclerosis process begins early in life (as early as teens in some people). When atherosclerosis is mild and the arteries are not substantially narrowed, atherosclerosis causes no symptoms. Therefore, many adults typically are unaware that their arteries are gradually accumulating cholesterol plaques. But when atherosclerosis becomes advanced with aging, it can cause critical narrowing of the arteries resulting in tissue ischemia (lack of blood and oxygen).
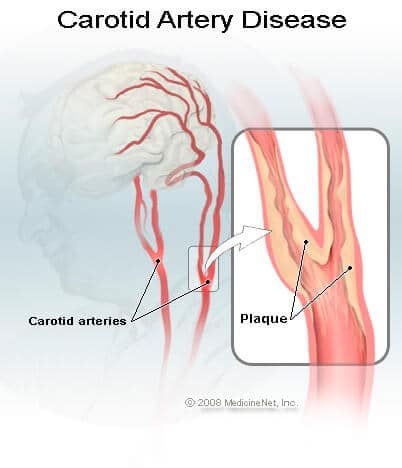
Arteries that are narrowed by advanced atherosclerosis can cause diseases in different organs. For example, advanced atherosclerosis of the coronary arteries (arteries that supply heart muscles) can lead to angina and heart attacks. Advanced atherosclerosis of the carotid and cerebral arteries (arteries that supply blood to the brain) can lead to transient ischemic attacks (TIAs) and strokes. Advanced atherosclerosis in the lower extremities can lead to pain while walking or exercising (claudication), deficient wound healing, and/or leg ulcers. Atherosclerosis is often generalized, meaning it affects arteries throughout the body. Therefore, patients with heart attacks are also more likely to develop strokes and peripheral vascular disease, and vice versa.
How does atherosclerosis cause symptoms?
There are two ways atherosclerosis causes disease; (1) atherosclerosis can limit the ability of the narrowed arteries to increase delivery of blood and oxygen to tissues during periods of increased oxygen demand such as during exertion, or (2) complete obstruction of an artery by a thrombus or embolus (thrombus and embolus are forms of blood clots; see below) resulting in tissue necrosis (death of tissue) if there are not enough collaterals. Exertional angina and intermittent claudication are two examples of insufficient delivery of blood and oxygen to meet tissue demand; whereas strokes and heart attacks are examples of death of tissue caused by complete artery obstruction by blood clots.
There are many similarities between coronary artery disease (atherosclerosis involving the arteries of the heart) and peripheral artery disease, and the two conditions may coexist in the same individual. For example, patients with exertional angina typically have no symptoms at rest. But during exertion the critically narrowed coronary arteries are incapable of increasing blood and oxygen delivery to meet the increased oxygen needs of the heart muscles. Lack of blood and oxygen causes chest pain (exertional angina). Exertional angina typically subsides when the patient rests. In patients with intermittent claudication, the narrowed arteries in the lower extremities (for example, a narrowed artery at the groin) cannot increase blood and oxygen delivery to the calf muscles during walking. These patients experience pain in the calf muscles that will only subside after resting.
Patients with unstable angina have critically narrowed coronary arteries that cannot deliver enough blood and oxygen to the heart muscle even at rest. These patients have chest pain at rest and are at imminent risk of developing heart attacks. Patients with severe artery occlusion in the legs can develop rest pain (usually in the feet). Rest pain represents such severe occlusion that there is insufficient blood supply to the feet even at rest. They are at risk of developing foot ulcers and gangrene.
When the arteries are narrowed as a result of atherosclerosis, blood tends to clot in the narrowed areas, forming a so-called thrombus (plural thrombi). Sometimes pieces of the thrombi break off and travel in the bloodstream until they are trapped in a narrower point in the artery beyond which they cannot pass. A thrombus or piece of thrombus that travels to another point is called an embolus. Thrombi and emboli can cause sudden and complete artery blockage, leading to tissue necrosis.
For example, complete blockage of a coronary artery by a thrombus causes heart attack, while complete blockage of a carotid or cerebral artery causes ischemic stroke. Emboli originating from atherosclerosis in the aorta (the main artery delivering blood to the body) can obstruct small arteries in the feet, resulting in painful and blue (cyanotic) toes, foot ulcers, and even gangrene.
What are collaterals?
Sometimes, despite the presence of a severe blockage in an artery, the involved area does not become painful or ischemic due to the presence of collateral vessels. Collateral circulation means that the particular area is supplied by more than one artery to an extent that blockage of a single vessel does not result in a severe degree of ischemia. Collateral circulation can develop over time to help provide oxygenated blood to an area where an artery is narrowed or occluded. Doctors believe that regular supervised exercise can stimulate the growth and development of collateral circulation and relieve symptoms of intermittent claudication.
What are potential complications of peripheral artery disease?
In severe cases, the decreased circulation to the extremities can lead to open sores that do not heal, ulcers, gangrene, or other injuries to the extremities. These areas that do not receive adequate blood flow are also more prone to develop infections and, in extreme cases, amputation may be necessary.
What are the other causes of peripheral vascular diseases?
A number of conditions such as vasculitis (inflammation of the blood vessels, occurring either as a primary condition or associated with connective tissue diseases such as lupus) may cause damage to blood vessels throughout the body. Injuries to blood vessels (from accidents such as auto accidents or sports injuries), blood-clotting disorders, and damage to blood vessels during surgery can also lead to tissue ischemia.
Tissue ischemia can also occur in the absence of atherosclerosis or other abnormalities of arteries. One example of a condition in which the blood vessels themselves are not damaged is Raynaud’s disease, which is believed to occur due to spasms in blood vessels brought on by stress, tobacco smoking, or a cold environment.
Optimized by: Netwizard SEO





