Peripheral Artery Disease and It’s Treatment
20 December 2020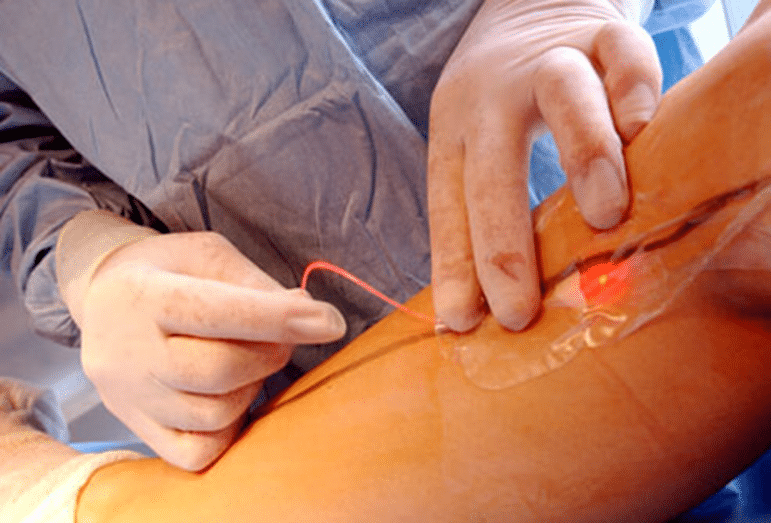
Peripheral artery disease (or peripheral arterial disease) is a common condition that affects approximately ten million adults in the U.S. About 5% of people over the age of 50 are believed to suffer from peripheral artery disease. Peripheral artery disease is slightly more common in men than in women and most often occurs in older persons (over the age of 50). The known risk factors for peripheral artery disease are those that predispose to the development of atherosclerosis. Risk factors for peripheral artery disease include:
- High blood levels of the bad LDL cholesterol and triglycerides
- Low blood levels of the good HDL cholesterol
- Cigarette smoking
- Diabetes mellitus (both type 1 and type 2 diabetes)
- High blood pressure (hypertension) or a family history of hypertension
- A family history of atherosclerotic disease
- Chronic renal failure
- Overweight or obesity
- Physical inactivity
In peripheral artery disease, the risk factors are additive, so that a person with a combination of two risk factors – diabetes and smoking, for example – has an increased likelihood of developing more severe peripheral artery disease than a person with only one risk factor.
What are the symptoms and signs of peripheral artery disease?
Approximately half of people with peripheral artery disease do not experience any symptoms. For patients with symptoms, the most common symptoms are intermittent claudication, and rest pain in more severe cases.
Intermittent claudication refers to arm or leg pain or cramping that occurs with exercise and subsides with rest. The severity and location of the pain of intermittent claudication can vary depending upon the location and extent of blockage of the involved artery. The most common location of intermittent claudication is the calf muscle of the leg, leading to leg pain while walking. The pain in the calf muscle occurs only during exercise such as walking, and the pain steadily increases with continued walking until the patient has to stop due to intolerable pain. Then the pain quickly subsides during rest. Intermittent claudication can affect one or both legs. Rest pain occurs when the artery occlusion is so critical that there is not enough blood and oxygen supply to the lower extremities even at rest and represents a more serious form of the condition. The pain typically affects the feet, is usually severe, and occurs at night when the patient assumes a supine position (lying down, face up).
Other symptoms and signs of peripheral artery disease include:
- Numbness of the extremities
- Weakness and atrophy (diminished size and strength) of the calf muscle
- A feeling of coldness in the legs or feet
- Changes in color of the feet; feet turn pale when they are elevated, and turn dusky red in dependent position
- Hair loss over the dorsum of the feet and thickening of the toenails
- Painful ulcers and/or gangrene in tissue where there is critical ischemia, typically in the toes
How is peripheral artery disease diagnosed?
During a physical examination, the doctor may look for signs that are indicative of peripheral artery disease, including weak or absent artery pulses in the extremities, specific sounds (called bruits) that can be heard over the arteries with a stethoscope, changes in blood pressure in the limbs at rest and/or after exercise (treadmill test), and skin color and nail changes due to tissue ischemia.
In addition to the history of symptoms and the physical signs of peripheral artery disease described above, doctors can use non-invasive and invasive tests in the diagnosis of peripheral artery disease. These tests include:
- Doppler ultrasound – This form of ultrasound (measurement of high-frequency sound waves that are reflected off tissues) can detect and measure blood flow. Doppler ultrasound is used to measure blood pressures behind the knees and at the ankles. In patients with significant peripheral artery disease in the legs, the blood pressures in the ankles will be lower than the blood pressure in the arms (brachial blood pressure). The ankle-brachial index (ABI) is a number derived from dividing the ankle blood pressure by the brachial blood pressure. An ABI of 0.9 to 1.3 is normal, an ABI less than 0.9 indicates the presence of peripheral artery disease in the arteries in the legs, and an ABI below 0.5 usually indicates severe arterial occlusion in the legs.
- Duplex ultrasound – This is a colour assisted non-invasive technique to study the arteries. Ultrasound probes can be placed on the skin overlying the arteries and can accurately detect the site of artery obstruction as well as measure the degree of stenosis.
- Angiography – A peripheral angiography is an imaging procedure to study the blood vessels of the extremities, similar to the way a coronary angiogram provides an image of the blood vessels supplying the heart. It is the most accurate test to detect the location(s) and severity of artery occlusive disease, as well as collateral circulations. Small hollow plastic tubes (catheters) are advanced from a small skin puncture at the groin (or the arm), under X-ray guidance, to the aorta and the arteries. Iodine contrast “dye”, is then injected into the arteries while an X-ray video is recorded. An Angiogram gives the doctor a picture of the location and severity of narrowed or occluded artery segments. This information is important in helping the doctor select patients for angioplasty or surgical bypass.
- Because X-ray angiography is invasive with potential side effects (such as injury to blood vessels and contrast reactions), it is not used for initial diagnosis of peripheral artery disease. It is only used when a patient with severe peripheral artery disease symptoms is considered for angioplasty or surgery. A number of different imaging methods have been used in angiography examinations, including X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scans.
- Magnetic resonance imaging (MRI) angiography uses magnetism, radio waves, and a computer to produce images of body structures and has the advantage of avoiding X-ray radiation exposure.
What are the treatments for peripheral artery disease?
Treatment goals for peripheral artery disease include:
- Relieve the pain of intermittent claudication.
- Improve exercise tolerance by increasing the walking distance before the onset of claudication.
- Prevent critical artery occlusion that can lead to foot ulcers, gangrene, and amputation.
Treatment of peripheral artery disease includes lifestyle measures, supervised exercises, medications, angioplasty, and surgery.

Lifestyle changes
Smoking cessation eliminates a major risk factor for disease progression and lowers the incidences of rest pain and need for amputations. Smoking cessation is also important for the prevention of heart attacks and strokes.
A healthy diet can help lower blood cholesterol and other lipid levels and may help control blood pressure.
Keep other risk factors, such as diabetes, lipid levels, and blood pressure under control by following medical advice regarding medications and lifestyle changes.
Supervised exercise
Proper exercise can condition the muscles to use oxygen effectively and can speed the development of collateral circulation. Clinical trials have demonstrated that regular supervised exercise can reduce symptoms of intermittent claudication and allow the patients to walk longer before the onset of claudication. Ideally, exercise programs should be prescribed by the doctor. Patients should be enrolled in rehabilitation programs supervised by healthcare professionals such as nurses or physiotherapists. For optimal results, patients should exercise at least three times a week, each session lasting longer than 30 to 45 minutes. Exercise usually involves walking on a monitored treadmill until claudication develops; walking time is then gradually increased with each session. Patients are also monitored for the development of chest pain or heart rhythm irregularities during exercise.
Peripheral vascular disease medications
While lifestyle changes may be enough treatment for some people with peripheral artery disease, others may require medication. Examples of medications used to treat peripheral artery disease include antiplatelet or anticlotting agents, cholesterol-lowering drugs, medications that increase blood supply to the extremities such, and medications that control high blood pressure.
Angioplasty for peripheral vascular disease
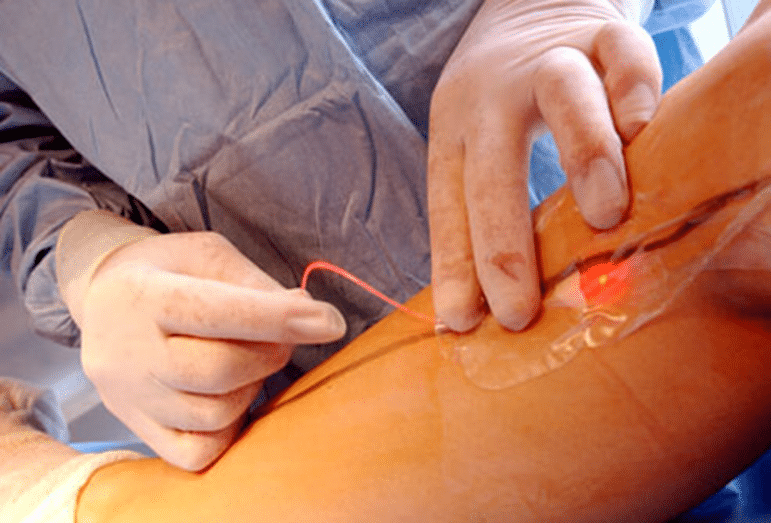
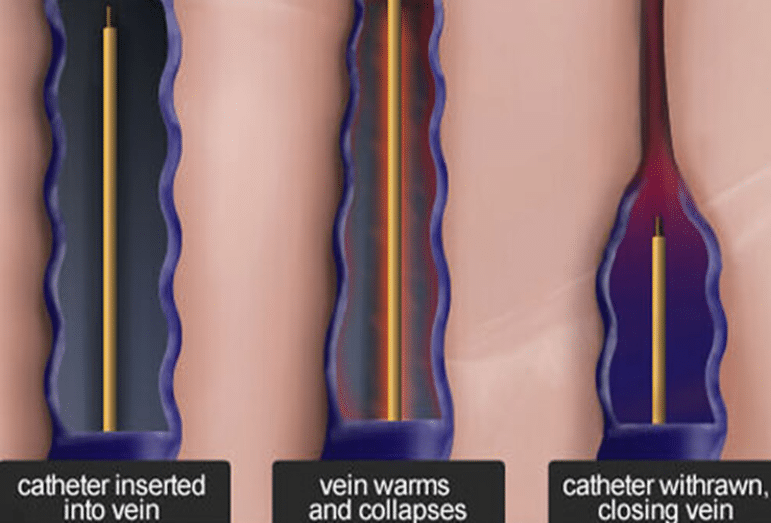
Angioplasty is a non-surgical procedure that can widen a narrowed or blocked artery. A thin tube (catheter) is inserted into an artery in the groin or arm and advanced to the area of narrowing. A tiny balloon on the tip of the catheter is then inflated to enlarge the narrowing in the artery. This procedure is also commonly performed to dilate narrowed areas in the coronary arteries that supply blood to the heart muscle.
Sometimes the catheter technique is used to insert a stent (a cylindrical wire mesh tube) into the affected area of the artery to keep the artery open. In other cases, thrombolytic medications (medications that dissolve blood clots) may be delivered to the blocked area via a catheter.
Angioplasty does not require general anesthesia and may be performed by an interventional radiologist, cardiologist, or vascular surgeon. Usually, a local anesthetic at the area of catheter insertion and a mild sedative are given. Major complications of angioplasty are rare but can occur. These include damage to the artery or blood clot formation, excessive bleeding from the catheter insertion site, and abrupt vessel closure (blockage of the treated area occurring within 24 hours of the procedure).
Despite these risks, the overall incidence of complications is low and the benefits of angioplasty (no general anesthesia, no surgical incision, and the ability to return to normal activities within a couple of days) outweigh its risks. Usually a one-night hospital stay is required when angioplasty is performed.
Angioplasty is indicated when a patient has claudication that limits his or her activities and does not respond to exercise, medications, and lifestyle measures. Angioplasty usually has a better outcome when disease is focal and accessible via catheter. If a patient is too ill to have surgery and has severe ischemia (decreased oxygen) that threatens loss of a limb, angioplasty may also be attempted.
Some cases of peripheral artery disease may be more difficult to treat by angioplasty. For example, blockages in multiple small arteries of the legs or blockages in extremely small vessels may not be treatable by this method.
Surgery for peripheral vascular disease
Surgical treatment for peripheral artery disease involves either bypass surgery performed by a vascular surgeon or endarterectomy. Indications for surgical treatment of peripheral artery disease include lesions that, for anatomical reasons, may be difficult to treat by angioplasty. Examples include lesions covering long segments of a vessel, vessels with multiple narrowed areas, or long areas of narrowing. Bypass surgery involves using a vein from your body or a portion of synthetic vessel (known as grafts) to create a detour around the blockage. One end of the graft is sewn to the artery above the blockage and the other end is sewn below the blocked area. Blood flow is then able to bypass the area of narrowing or blockage. Bypass surgery is a major surgical procedure requiring general anesthesia and a hospital stay. Endarterectomy is a procedure in which the surgeon cleans out plaque buildup inside the artery of the affected leg or arm.
Optimized by: Netwizard SEO





