Raynaud’s Syndrome Diagnosis
What is Raynaud’s Syndrome?
Raynaud’s Syndrome is a disorder of the blood vessels, usually in the fingers or toes, causing blood vessels to narrow when exposed to cold temperatures or during periods of stress. This narrowing, or vasoconstriction, leads to reduced blood perfusion to the affected sites.
This condition is also known as Raynaud’s Disease or Primary Raynaud’s when not accompanied by arterial obstruction. In cases where it is accompanied by arterial obstruction, it is referred to as Raynaud’s Phenomenon or Secondary Raynaud’s.
The terms “Raynaud’s syndrome,” “Raynaud’s disease,” “Raynaud’s phenomenon,” and “Raynaud’s disorder” are often used interchangeably.
When Raynaud’s occurs, blood cannot reach the surface of the skin, resulting in areas turning white or blue. In severe cases, this reduced blood flow can lead to sores or tissue death.
Prevalence and Risk Factors of Raynaud’s Syndrome
Raynaud’s Syndrome affects approximately 5% of the population, with a higher occurrence in females. It is more prevalent in regions with cold climates.
The risk factors for this condition include smoking and alcohol consumption.
How to Test for Raynaud’s
To diagnose Raynaud’s Disease, physiological tests are typically performed. Such tests include measuring of photoplethysmography (PPG) waveforms with or without blood pressure in the fingers or toes, both at room temperature and after cold immersion.
Here is an example of a step-by-step guide for performing Raynaud’s Syndrome Test:
- Preparation: Ensure a suitable testing environment with controlled temperature conditions. Make sure the room temperature is comfortable and consistent throughout the test.
- Explanation and Consent: Explain the procedure to the patient, including its purpose and potential sensations they might experience during the test. Obtain informed consent from the patient before proceeding.
- Positioning: Ask the patient to sit in a relaxed position, with their hands or feet comfortably placed on a surface.
- Baseline Measurement: Before any cold exposure, measure the patient’s baseline photoplethysmography (PPG) waveform and/or blood pressure in the fingers or toes at room temperature. Record these measurements as the baseline values for later comparison.
- Cold Immersion: Remove the PPG sensor from the patient’s digits or toes. Prepare a container filled with cold water. Ask the patient to immerse their hand or foot (depending on the area being tested) into the cold water for a specified duration. The cold immersion should be long enough to elicit a response but not to the point of discomfort or pain.
- Observation and Measurements: While the hand or foot is immersed in cold water, closely observe the color changes in the affected area. Note any visible signs of blanching or discoloration.
- Recovery Period: After the specified cold immersion duration, instruct the patient to remove their hand or foot from the cold water and allow it to return to room temperature. Reattach the PPG sensors and measure the recovery of the PPG waveforms or blood pressure as the affected area returns to its baseline state.
- Analysis and Interpretation: Compare the PPG waveforms or blood pressure measurements taken during the cold immersion and the recovery period with the baseline values. Look for any significant changes, such as delayed recovery or abnormal patterns, which may indicate Raynaud’s Syndrome or other related conditions.
- Documentation and Reporting: Record the test results accurately, including the measurements, observed responses, and any notable observations. Prepare a comprehensive report summarizing the findings and interpretations for further analysis or consultation with a healthcare professional.
Remember, this step-by-step guide is a general outline for performing a Raynaud’s test. The specific protocol may differ among hospitals and institutions. Healthcare professionals should follow appropriate protocols based on their expertise and available resources.

PPG Sensors
Required for Raynaud’s Assessment

Inflatable Cuffs
Optional Method for Raynaud’s Diagnosis
Using the Falcon for Raynaud’s Measurements
The Falcon/PRO system offers significant advantages for Raynaud’s diagnosis:
- Enhanced Efficiency: The Falcon/PRO vascular machine offers dedicated protocols for Raynaud’s testing, allowing for rapid and simultaneous measurement of photoplethysmography (PPG) waveforms and systolic blood pressure in all five fingers or toes at the same time. This significantly reduces the time and effort required for performing the test compared to traditional methods that require separate measurements for each digit.
- Improved Patient Experience: The Falcon/PRO system’s design eliminates the need for patients to repeat the cumbersome and sometimes painful process of immersing each finger or toe individually in cold water. With the Falcon/PRO system, the patient only needs to immerse their hand or foot in cold water once, enhancing comfort and convenience during the examination.
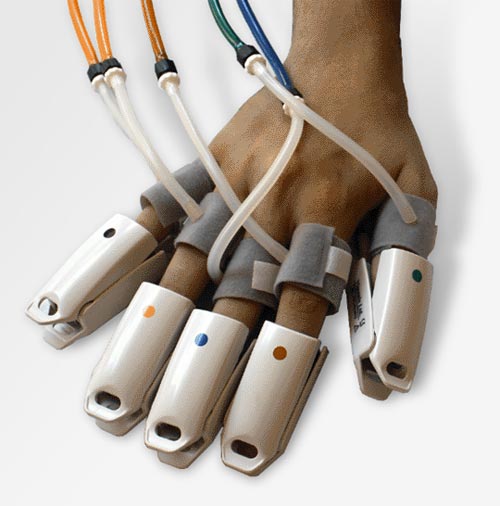
- Comprehensive Measurements: The Falcon/PRO machine is equipped with five color-coded PPG sensors and ten independent pressure channels, ensuring detailed measurements of PPG waveforms and systolic blood pressure. These measurements provide valuable information for diagnosing Raynaud’s Phenomenon and help in assessing the severity of the condition.
- Integrated Temperature Monitoring: The Falcon/PRO machine includes an integrated temperature sensor, which plays a crucial role in documenting the skin temperature during cold immersion and continuously monitoring the skin temperature during the recovery period.
- Streamlined Analysis and Reporting: The Falcon/PRO system offers various print and report options specifically designed for a detailed comparison between pre- and post-immersion results. The system presents parameters such as PPG waveform amplitude, systolic rise time, and systolic blood pressure differences in a graphical manner, facilitating comprehensive analysis and highlighting potential pathology.
By utilizing the Falcon/PRO system’s advanced capabilities, healthcare professionals can benefit from a comprehensive and efficient diagnostic workflow. The system’s simultaneous measurement of multiple parameters and its ability to capture detailed data provide a more robust diagnosis and improved treatment planning.
Expected Results
During a Raynaud’s Syndrome test, several expected results and observations can be noted. First, during the cold immersion phase, the affected area may exhibit color changes, turning white or blue due to vasoconstriction and reduced blood flow. This discoloration serves as a characteristic sign of Raynaud’s Syndrome.
Additionally, the focus of the test is on the time it takes for the PPG waveforms to return to their pre-immersion amplitude levels after exposure to cold temperatures.
It is expected that the PPG waveforms will gradually recover and return to their baseline levels within approximately 10 minutes or so. This recovery time can vary depending on individual factors and the severity of the condition. A longer duration for the waveforms to return to pre-immersion levels may indicate the presence of a disease condition related to Raynaud’s Phenomenon.
Systolic blood pressure measurements can provide further insights into the diagnosis. In cases of secondary Raynaud’s, a decrease in systolic blood pressure compared to primary Raynaud’s is typically observed. This difference in blood pressure readings can help distinguish between primary and secondary forms of the condition.
To summarize, the expected results of a Raynaud’s Syndrome test include color changes in the affected area, gradual recovery of the PPG waveforms to their baseline levels within approximately 10 minutes, and potential variations in systolic blood pressure readings between primary and secondary Raynaud’s cases. These observations serve as important indicators for diagnosing and assessing the condition.
Selected Literature
Wigley FM. Clinical practice. Raynaud’s Phenomenon. N Engl J Med. 2002;347(13):1001-1008.
Assessment of upper extremity arterial occlusive disease, Steven R. Talbot, in “Introduction to Vascular Ultrasonography”, Ed. Pellerito and Polak, Elsevier Health Sciences, 2012, Ch 15, pp 262-280
Herrick AL. Pathogenesis of Raynaud’s phenomenon. Rheumatology (Oxford). 2005 May;44(5):587-96
Three-Grade Classification of Photoplethysmography for Evaluating the Effects of Treatment in Raynaud Phenomenon, Shin-Seok Yang et al., Angiology 64(8) 609-613, 2012
Multifinger photoplethysmography and digital blood pressure measurement in patients with Raynaud’s phenomenon of the hand, J H Tordoir, L B Haeck, H Winterkamp, W Dekkers, J Vasc Surg, 1986 Mar;3(3):456-61.
What is Thoracic Outlet Syndrome?
The Thoracic Outlet Syndrome test (TOS) is an examination performed primarily to discriminate between the causes of patient symptoms due to compression at the thoracic outlet. The compression can affect the blood vessels or nerves, and the TOS test is conducted to determine whether the patient symptoms originate from vascular or neurogenic causes.
How to Perform Thoracic Outlet Syndrome Test
This diagnostic vascular TOS procedure tests for intermittent perfusion loss, particularly in the arms and hands. Either Doppler, PVR, or PPG sensors can detect normal resting waveforms in the digits or hands. Then, the patient is instructed through a sequence of positional maneuvers, which include the symptomatic position.
The examination tries to identify a position that significantly reduces perfusion to determine whether the symptoms originate from a vascular disorder. The examination is typically performed in parallel on both the right and left sides.
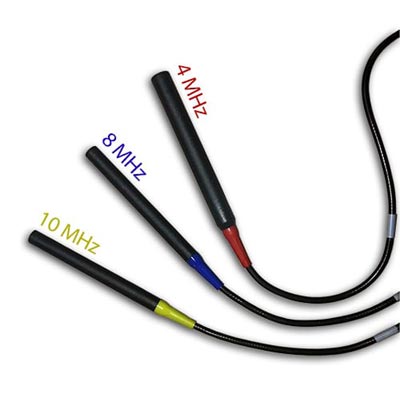
Doppler Probes
Gold Standard ABI Measurement Method

PPG Sensors
Secondary Method of ABI Assessment

Inflatable Cuffs
High quality available in a variety of sizes
Using the Falcon for TOS Assessment
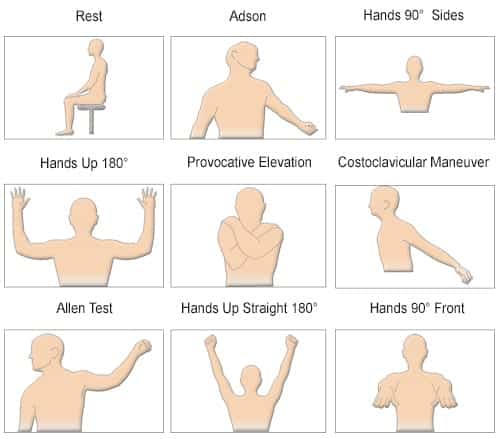
The Falcon is designed with a dedicated TOS protocol to allow a complete and effective diagnosis. The protocol guides both the examiner and the patient through a series of positional maneuvers that are visually presented with schematic pictures for clarity and to avoid mistakes. The range of positions includes maneuvers such as:
- Hands-up Test,
- Adson or Scalene Maneuver,
- Costoclavicular Maneuver,
- Allen Test,
- Provocative Elevation Test,
- And more.
However, additional maneuvers can be added, and the protocol can be easily configured accordingly. The symptomatic position, which is probably the most important maneuver, is also included in the protocol. The examiner can use the Falcon camera to take a picture of the symptomatic position and document it in the protocol and subsequent report.
While standard TOS requires the use of PPG sensors (photoplethysmography sensors), the Falcon also supports a complete range of TOS testing capabilities, including Doppler and PVR measurements. All sensors can be placed for maximal efficiency, for example, on both the right and left digits, and these sites will be measured simultaneously. For even more effective evaluation, up to 5 PPG sensors and 10 PVR waveforms (for each finger) can be measured simultaneously.
The diagnosis of the TOS test is primarily visual. Still, the Falcon also provides a range of quantitative parameters, including PPG and PVR waveform amplitudes and the Doppler parameters range. These quantitative measurements help to support the qualitative findings.
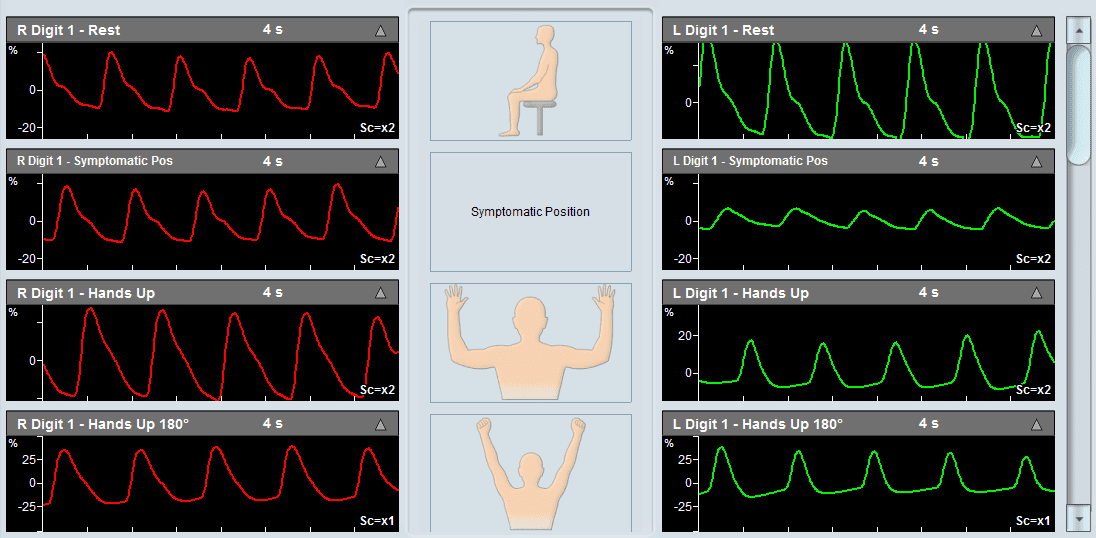
Expected Results
The diagnosis of the TOS test is primarily qualitative in nature. The focus is on viewing the measured waveforms on both the right and left sides for each positional maneuver and determining whether a specific position resulted in an abnormal decrease in amplitude or resulted in signal flattening. Such a case is indicative of a potential decrease in perfusion, suggesting a vascular source of TOS.
An example of a Thoracic Outlet Syndrome examination taken using Viasonix Falcon/PRO system.
Selected Literature
Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome, Karl A. Illig et al., J Vasc Surg 2016;64:e23-e35.
Diagnosis and Treatment of Thoracic Outlet Syndrome, Editors Julie Ann Freischlag and Natalia O. Glebova, 2018 MDPI, Basel, Switzerland
What are Palmar Arch Test and AV Fistula?
The Palmar Arch Test (PAT), also known as Allen’s Test, is a specialty test performed to evaluate the patency of the arteries in the hand prior to radial or ulnar artery harvesting in artery bypass procedures or before the surgical creation of an upper extremity hemodialysis fistula or graft.
How to Perform PAT (Allen’s Test)
The PAT procedure provides a clinical assessment of the collateral circulation to the hand to determine if arterial harvesting is possible. The test is quite simple and involves sequential compression of the radial and ulnar arteries, and determining the physiological effect on the blood flow circulation in the hand. The blood flow assessment can be performed by different means, with the most popular method being with PPG sensors (Photoplethysmography).
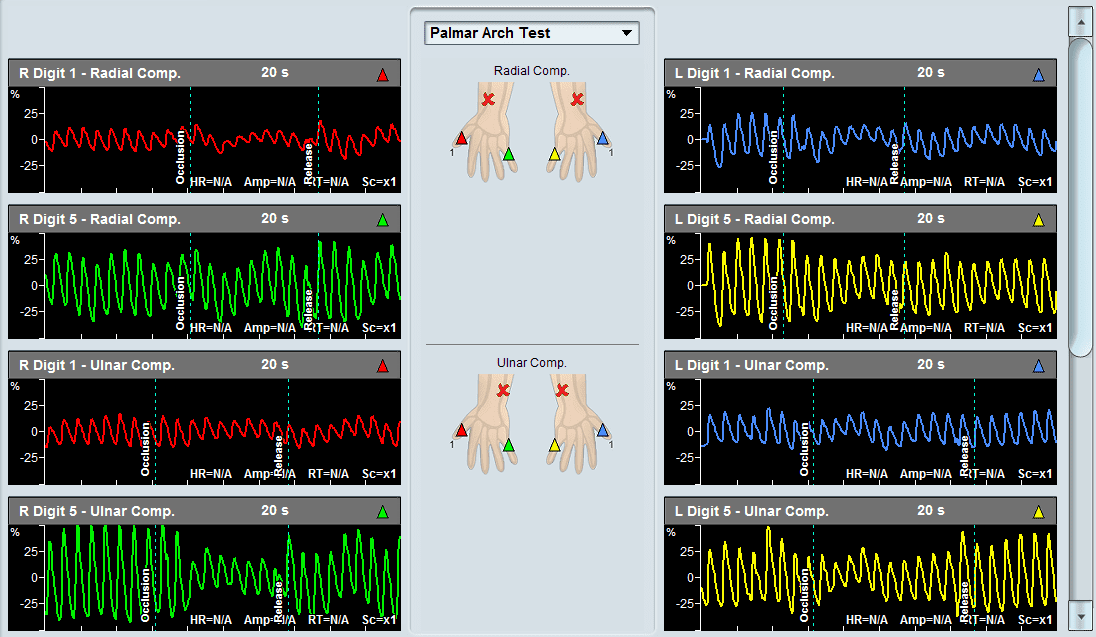
Additional diagnosis options include digit blood pressure measurements, PVR measurements (Pulse Volume Recording), and Doppler blood flow measurements. When using PPG sensors, it is preferred to use at least 2 PPG sensors, which are placed on the two extreme digits (digit 1 and digit 5). The Palmar Arch Test protocol begins by measuring the resting PPG waveforms, then measuring the waveforms after selected compressions (compression of the radial artery, ulnar artery, or both), and finally measuring the waveforms after the release of the selected compression. A similar protocol is applied when using digit pressure, Doppler, or PVR assessment.
Compression is typically performed by manually compressing the selected artery or arteries. This procedure allows the examiner to evaluate whether the result of the compression is impeded or complete loss of blood flow to parts of the hand. Thus, significant reduction or loss of blood flow to areas of the hand suggests that removing that particular artery may jeopardize hand performance if the artery is removed.

PPG Sensors
Secondary Method of ABI Assessment

Inflatable Cuffs
High quality available in a variety of sizes
Using the Falcon for PAT Measurements
The Falcon has a dedicated Palmar Arch Test (PAT) protocol, which is designed to complete the assessment in guided procedures per the accepted guidelines. While the standard clinical assessment is with PPG sensors on the 2 extreme digits, the Falcon has the ability to place a PPG sensor on each of the 5 digits and perform the test simultaneously for all digits for optimal clinical assessment. The Falcon also supports digit blood pressure measurements pre-, during and post-arterial compression.
In addition, digit Doppler and/or PVR measurements can be performed with the Falcon.
The PAT protocol includes schematic pictures, which help visualize to the examiner the required compression stage. The measured waveforms are clearly marked with automatic cursors to indicate when artery compression begins and when the compression is released. Thus, a quick visual assessment of the effect of compression on blood flow to the different parts of the hand is possible.
All sensors are color-coded, simplifying the interaction with the software. The ability to zoom in and out of the waveforms allows to quickly qualitatively determine whether a specific arterial compression has a patent collateral circulation or that harvesting the vessel will jeopardize the hand.
Expected Results of Palmar Arch Test
A decrease in the ipsilateral signal when compressing an artery, whether PPG waveform, blood pressure, PVR waveform, or Doppler spectrum, is indicative of impaired collateral circulation in the hand, and is generally considered as a contraindication to arterial harvesting.
For blood pressure assessment, a Finger Brachial Index (FBI) greater than 0.9 is considered normal. FBI is defined as the digit pressure divided by the ipsilateral brachial pressure. The determination of what is considered a significant drop in digit pressure varies in the literature but is in the range of a drop of 40 mmHg after radial/ulnar artery compression.
Example of a Palmar Arch Test specialty test performed on a patient using Viasonix Falcon/PRO. First, the Radial artery was compressed on two extreme digits, and then the Ulnar artery was compressed on the same digits.
Selected Literature on Palmar Arch Test
Preoperative Assessment of Hand Circulation by Means of Doppler Ultrasonigraphy and the Modified Allen Test, Permyos Ruengsakulrach et al., J Thorac Cardiovasc Surg 2001;121:526-31
Assessment of collateral circulation to the hand prior to radial artery harvest, Joseph Habib, Laureen Baetz and Bhagwan Satiani, Vascular Medicine 17(5) 352– 361
Allen Test, Jonah Zisquit; James Velasquez; Nicholas Nedeff, National Center for Biotechnology Information, U.S. National Library of Medicine, NCBI Bookshelf, StatPearls Publishing LLC., 2020





